Kymera’s IRAK4 degrader for hidradenitis suppurativa: Hitting an elusive target hard for a hard-to-treat inflammatory disease
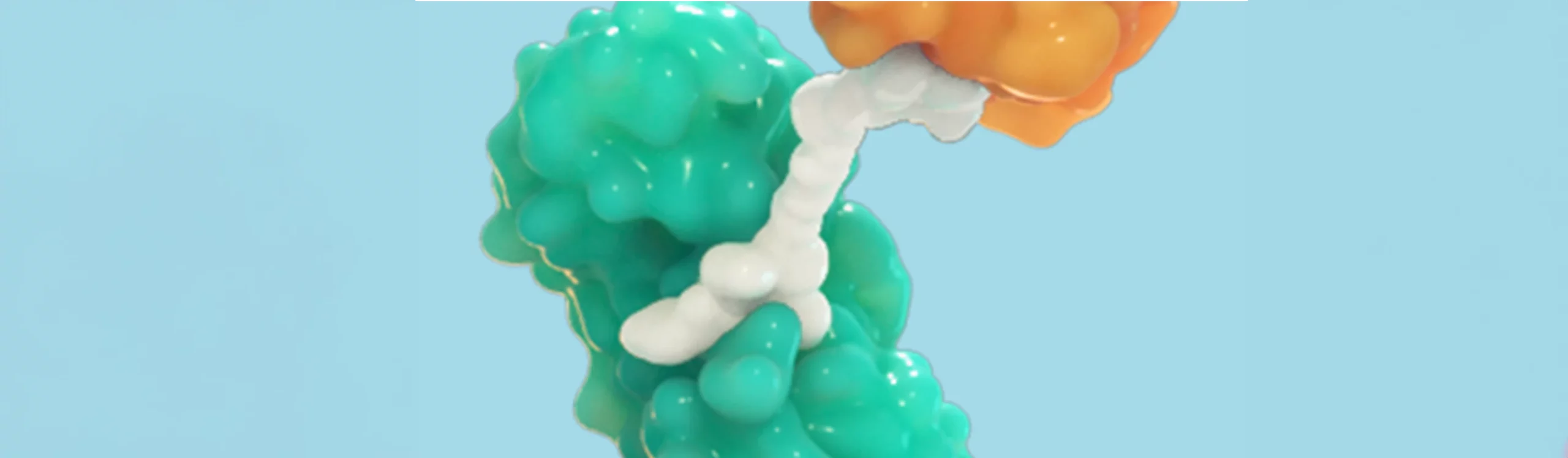
IRAK4 is a key component of the myddosome, a protein complex that transmits signals from toll-like receptors (TLRs) and IL-1 receptors (IL-1Rs) to activate the innate immune response to infectious pathogens. While TLR/IL-1R activation is ordinarily protective, aberrant activation is at the root of certain highly morbid and sometimes life-threatening inflammatory and autoimmune conditions, such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), atopic dermatitis (AD) and hidradenitis suppurativa (HS). Since myddosome signaling leads to the production of multiple different pro-inflammatory cytokines and chemokines that contribute to disease pathogenesis, targeting single cytokines with monoclonal antibodies has had limited efficacy. By contrast, shutting down the myddosome through IRAK4 targeting may enable a single drug to more effectively treat TLR/IL-1R-driven diseases.
In order to completely drug IRAK4 to block MYD88 downstream signaling, both its scaffolding and kinase functions must be removed, something which can only be accomplished through elimination of the protein. At Kymera, we chose to develop an IRAK4 degrader for precisely this reason, as we believed it offers the only approach to drugging the myddosome hard enough to be transformative for high unmet need inflammatory diseases caused by TLR activation and the effects of IL-1 family cytokines such as IL-1alpha, IL-1beta, IL-36, IL-18 and IL-33. The advantage of eliminating IRAK4 protein over just inhibiting its kinase function, also known as the degrader advantage, is evident in our preclinical models of inflammation where IRAK4 degraders but not kinase inhibitors most effectively block cytokine and chemokine induction by TLR agonists such as lipopolysaccharide (LPS) and imiquimod as well as LPS combined with IL-1beta in vitro in a context-independent manner, and also block neutrophil infiltration in the monosodium urate mouse air pouch model of gouty inflammation.
We now have a potent, highly selective, orally-administered IRAK4 degrader for the treatment of TLR- and IL-1 family cytokine-dependent diseases that has entered into IND-enabling studies with the goal of starting a Phase 1 study in healthy volunteers by Q4 of this year. The first indication being targeted is HS, a chronic, destructive, painful and debilitating inflammatory skin disease affecting up to 1% of the US population. The disease is usually diagnosed in the 3rd and 4th decades of life, affects women more than men (3:1 ratio), and is more common in African-Americans. Patients with HS have numerous painful, draining nodules and abscesses, usually within skin folds, that are characterized by neutrophilic inflammation and bacterial colonization. This is accompanied by signs and symptoms of systemic inflammation, including fatigue, depression and elevation of inflammatory biomarkers in the blood. HS is treated palliatively with corticosteroids, antibiotics and surgery. The only approved drug is the anti-TNF antibody Humira, which benefits approximately 50% of patients with moderate to severe disease but is not curative; thus, there is a high unmet need for better therapies for HS.
Bacterial activation of TLRs, as well as the production of IL-1beta and IL-36 by keratinocytes and inflammatory cells leading to the generation of Th1 and Th17 inflammation, are central to the pathogenesis of HS and the reason why targeting IRAK4 hard with a degrader holds great promise for the treatment of this disease. We have shown in preclinical studies in rodents and higher species that daily oral dosing of our degrader leads to complete knockdown of IRAK4 protein in skin, peripheral blood mononuclear cells, lymph nodes and spleen with a favorable safety profile. In the imiquimod-induced model of psoriasis in mice, which includes Th1 and Th17 cutaneous inflammation, Kymera’s IRAK4 degrader abrogates skin thickening and the in vivo production of IL-1beta, IL-17, IL-23 and IL-6. These encouraging results support development of in HS, with a Phase 2 proof of concept study planned for H2 2021 following the establishment of safety and on-target pharmacology in the Phase 1 healthy volunteer trial.
The demonstration of efficacy in HS will de-risk development in other Th1- and/or Th17-driven diseases such as RA, SLE and psoriasis, and enable exploration of additional opportunities in IL-33-driven diseases like AD and allergic asthma. Capitalizing on the degrader advantage for a target like IRAK4 to hit a key signaling node in inflammation also provides precedent for a second program at Kymera targeting STAT3. We have developed highly selective degraders for this previously undruggable transcription factor which serves as a key driver of Th17 inflammation as well as fibrosis, thereby providing the ability to hit hard another signaling node involved in a diverse array of hard-to-treat autoimmune and fibrotic diseases ranging from systemic sclerosis and inflammatory bowel disease to idiopathic pulmonary fibrosis.