IRAKIMiDs: A Single Small Molecule Approach to Developing Dual-Function Degraders for B Cell Lymphoma with Multiple Drivers
At this week’s American Association of Cancer Research virtual meeting, Kymera provided first disclosure of our IRAKIMiD program, which uses novel dual-function degraders for the treatment of diffuse large B cell lymphoma (DLBCL). In this post, I provide the rationale for the approach and the promising data we’re seeing in preclinical studies.
An aggressive hematologic malignancy, DLBCL is characterized by cellular proliferation and resistance to cell death mediated through activation of NF-kB signaling and IRF4-induced downregulation of the Type I Interferon response, respectively. A key driver of some forms of DLBCL is MYD88, a component of the multi-protein myddosome complex which normally mediates innate immune signaling through toll-like receptors (TLRs) and interleukin-1 receptors (IL-1Rs) but is constitutively activated through oncogenic mutations in up to 35% of nodal activated B cell-type (ABC) DLBCL and up to 80% of primary extranodal lymphomas, including primary CNS lymphoma. IRAK4 is necessary for myddosome assembly and signaling following MYD88 activation and therefore represents a rationale target to drug. However, lymphomas with MYD88 mutations also commonly have co-mutations in CD79B, TNFAIP3, and/or CARD11 that further increase NF-kB activation and suppression of the Type I Interferon response, thereby limiting the effectiveness of single agents that target either NF-kB signaling (e.g. IRAK4 kinase inhibitors, BTK inhibitors) or the Type I Interferon response (e.g. IMiDs such as lenalidomide).
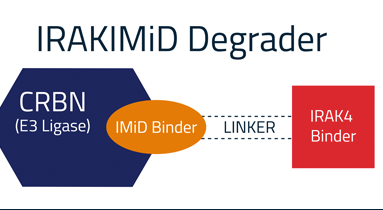
Targeted protein degradation (TPD) is a promising new modality that involves the use of heterobifunctional small molecules to bring an E3 ligase and protein target of interest together in a ternary complex, leading to ubiquitination and subsequent proteasomal degradation of the target. We viewed TPD as the optimal way to fully drug IRAK4 as both its kinase function and scaffolding function are necessary for myddosome assembly and signaling.
We have demonstrated through in vitro and in vivo studies that by degrading and removing the IRAK4 protein, thereby impacting both the kinase and the scaffolding functions of IRAK4, we can potently and selectively block IL-1R/TLR-mediated signaling in a way we believe to be superior to what can be achieved with IRAK4 kinase inhibitors. This underscores the importance of eliminating the protein to fully realize the therapeutic potential of IRAK4 targeting.
In DLBCL, IMiDs such as lenalidomide have also been shown to inhibit the activation of NF-kB signaling while promoting Type I Interferon responses. Therefore, we hypothesized that the degradation of both IRAK4 and IMiD substrates had the potential for superior activity relative to either approach alone. Early in vitro data showing synergistic activity of an IRAK4 degrader and an IMiD provided the key rationale for our IRAKIMiD program.
Leveraging knowledge and chemistry expertise derived from the design of our selective IRAK4 degrader program, we have designed a novel class of heterobifunctional IRAK4 degraders, which we call IRAKIMiDs. These are protein degrader therapies comprised of an IRAK4-targeting ligand coupled to an IMiD that binds to the E3 ligase cereblon (CRBN). As a component of IRAKIMiDs, this IMiD serves two functions. First, it brings CRBN into proximity with IRAK4, thereby enabling the ubiquitination and subsequent degradation of IRAK4. Secondly, through its interaction with CRBN, it also recruits the neosubstrates Ikaros and Aiolos, two zinc-finger transcription factors with immunomodulatory effects including the upregulation of IRF4, and leads to their ubiquitination and subsequent degradation. This results in the combined degradation of IRAK4, Ikaros and Aiolos, which in turn shuts off NF-kB activation and turns on the Type I Interferon response via IRF4 downregulation, resulting in increased and broader single-agent activity in MYD88-mutated DLBCL as compared to either mechanism alone.

Data presented at AACR show the remarkable potency of IRAKIMiDs against both IRAK4 and IMiD substrates Ikaros and Aiolos, as well as the breadth and depth of responses across multiple MYD88-mutant DLBCL cell lines with various co-mutations in CD79B and TNFAIP3 that were superior to IMiDs (including the newer, more potent compounds in development) and an IRAK4 kinase inhibitor. Notably, IRAKIMiDs induced robust tumor regressions in multiple mouse xenograft models of MYD88-mutant lymphoma associated with >80% reduction of IRAK4 and IMiD substrates in tumors. These findings were remarkable, since active agents in DLBCL like BTK inhibitors and IMiDs show varying degrees of tumor growth inhibition but not regression in preclinical models.
These compelling preclinical data demonstrate the potential of dual-targeting IRAKIMiDs to transform the treatment of a genetically-defined subset of DLBCL through the inhibition of two pathways that are affected by MYD88 mutations as well as by co-mutations frequently found in these patients. IRAKIMiDs also demonstrate the versatility of heterobifunctional protein degraders and the various ways in which E3 ligases can be rationally paired with high impact targets of interest to elicit the best pharmacological responses and thereby, optimally drug key pathways involved in disease pathogenesis. The novelty of this approach, impressive preclinical antitumor activity, and the potential to provide a stand-alone therapy with the ability to address tumor escape mechanisms in DLBCL have generated considerable enthusiasm from an international group of lymphoma KOLs as well as support from the Leukemia and Lymphoma Society through its Therapy Acceleration Program. Our lead compound is on track for a Phase 1 trial in relapsed/refractory B cell lymphoma patients, including MYD88-mutant DLBCL, starting in 2021.